Cess Now?
Confusion and panic greet respiratory therapist student dropping his first tube
“You, come here.” Head whipping around, I looked desperately for the person I hoped to see standing behind me. It took about half a second to realize my savior wasn’t there and that the ER doctor meant me. If I were a puppy, I’d have peed on the floor.
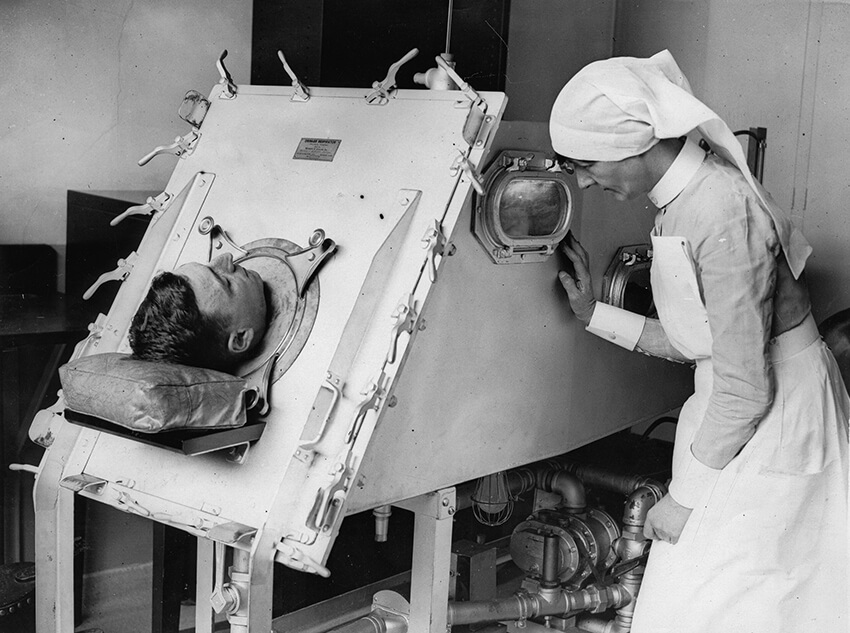
Covid-19 has brought many new words and phrases front and center in the American lexicon: Zoom meeting, social distance, ventilator….
Early in the pandemic, New York’s Gov. Cuomo said that if his state didn’t receive thousands of these devices, there would be mass carnage. General Motors, Philips, and other manufacturers turned their resources toward producing these machines, and ventilators became ubiquitous, if not always at health care facilities at least in our language.
Ventilators might put on a complex front with their plethora of lights, screens, and graphs, but at their heart, they are compressors that push air in and allow air out, albeit in highly specific ways. The truly complicated part of operating a ventilator is when one’s connected to that most distinct of variables: the patient. This is where I come in, a respiratory therapist, more commonly known as an RT.
When it comes to health care professionals, everyone is familiar with doctors and nurses, but branch out into what is known as “allied health” and familiarity starts to fade. Allied health includes health professionals such as radiology technicians, laboratory technicians, and others who work in direct clinical care but are not physicians, nurse practitioners, physician assistants, or nurses. As a respiratory therapist, I earned a two-year Associates of Science before sitting for three national examinations to earn my credentials.
Since Covid-19, RTs’ profiles have risen. Vents aren’t all we do. RTs also manage the airway during traumas in the emergency room, provide aid with neonatal resuscitation during deliveries, treat patients in asthmatic crises, and handle a host of other pulmonary-related issues. As we like to say, “If the patient isn’t breathing, they’re not doing much of anything else, either.”
Forty-five minutes before being summoned by the emergency department attending doctor at Maine Trauma Center, I had put on hospital scrubs for the first time in my life. How a 50-year-old ended up a student in the respiratory therapy program at Katahdin River Community College is another story, but suffice it to say, this wasn’t what I thought my first day of clinicals would be like. Hell, I didn’t even know where the bathrooms were and was pretty sure I’d parked my car in a tow-away zone.
Clinical rotations, or clinicals, are the practical, manual part of training in medical education programs. To bolster classroom instruction, doctors, nurses, certified nursing assistants, radiology technicians, and, yes, respiratory therapists all spend varying amounts of time, from weeks to years, in hospitals, nursing homes, clinics, or doctors’ offices getting hands-on experience with real patients.
KRCC began students’ clinical rotations in the summer between the first and second year. We were given two weeks off following our completion of year one, so clinicals for me began the day after Memorial Day weekend. We were told to be dressed and ready to go for the 6:45 a.m. shift change report. And so it was in the wee small hours of that fateful Tuesday morning I got out of my 10-year-old Hyundai, threw my backpack over one shoulder, and made my way toward MTC.
* * *
At Maine Trauma, everyone in the same discipline, even students, wore the same color scrubs, all provided by the hospital. Nurses wore navy blue; for radiology techs it was gray; and the respiratory therapy department wore what was believed to have been, at least at some point, maroon. Over time and hundreds of industrial washings, they had morphed into some sort of a pink/magenta. Students wore the same nametags as the professionals, the sole exception a bright orange band across the bottom with black letters proclaiming “STUDENT.” There were five of us my first day, and once we had all changed we made our way to the respiratory department and morning rounds.
The department manager, Sarah, was on hand to introduce us and assign each of us a preceptor for the shift. Preceptors are the one-on-one instructors/babysitters/psychologists assigned to ride herd on each student for a day. Like anything else, there are some folks who excel in the role, others not so much. My preceptor that day was an RT named Ned. Ned seemed like a nice guy: big smile, hearty handshake, lots of “us” and “we” talk. I thought I had hit the preceptor jackpot.
Unfortunately, Ned was a traveler, and today was the last day of his contract. Travelers, who represent many medical disciplines, work for companies that fill temporary staffing shortages at hospitals. They typically work 13-week contracts and then move on to another facility or stay on for another contract if the need is still there. Ned had finished his commitment to MTC and was moving on to a new assignment the following day. I’m not saying that Ned was shirking his duties, but he just might have been a little more relaxed than normal.
Halfway through report, Ned’s pager went off. Staring at the screen, he announced, “They’re dropping a tube on the MVA in ED 34. Grab your stuff, Mike. Let’s move.” I wasn’t exactly sure which stuff I was supposed to grab. Death-gripping my bright, shiny new stethoscope, I lit out after Ned on my way to the crème de la crè me of RT student experiences, the intubation.
An intubation, or “dropping a tube,” is the process by which a flexible plastic tube is inserted into the airway of a person who is, for whatever reason, no longer able to breathe reliably for themselves. In some situations the RT will do the intubation; in others they will assist the physician, nurse practitioner, or physician assistant; but almost always, once the tube is in, it is the RT’s province to secure it and further manage the airway.
* * *
MTC is a teaching facility, so there was a pretty good crowd of students and preceptors gathered by the time Ned and I arrived to the room in the emergency department. I was able to find an open area near the door and, being a little taller than the rest of the group, had a decent vantage point. The patient was an 81-year-old man who had been in an automobile accident. Dr. Powell, the attending that day, was at the head of the bed and flanked on his right by one of the ED interns and on his left by Angela, one of the MTC staff RTs.
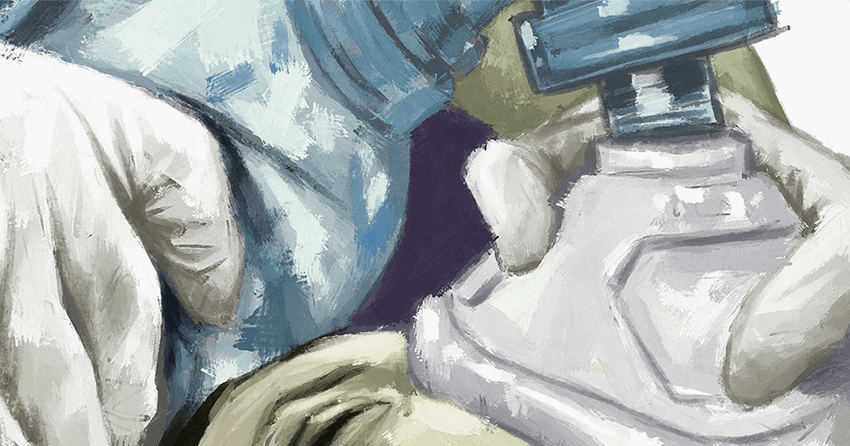
This was my first intubation, my first procedure of any kind for that matter, and I was having my initial run-in with reality. The tidy photos in my Egan’s Fundamentals of Respiratory Care textbook had been replaced by an octogenarian lying on his back on a stretcher, his dentures, an endotracheal (or ET) tube, and a laryngoscope perched on his chest. Angela calmly administered oxygen and positive pressure with an Ambu bag, a device squeezed by hand that allows a volume of air, oxygen, or a mixture of the two to be given under varying amounts of pressure through a mask or an ET tube. Meanwhile, the doctor gave medication orders to the nursing staff. Intubation is a singularly unpleasant experience for the patient, so a series of four medications are typically given for anxiety, pain, sedation, and, finally, to act as a paralytic.
There are numerous paralytics used when intubating a patient, two of the more common being rocuronium and succinylcholine — “rock” and “sux.” While they have different methods of action and longer or shorter durations of effectiveness, all share one commonality: They paralyze the muscles involved in breathing. If an individual were to have one of these medications administered and everyone walked away, the patient would suffocate within a few minutes.
Satisfied that everything was ready, Dr. Powell ordered the paralytic be given, and following an appropriate wait I saw him crouch over the patient’s head, insert the laryngoscope into the his open mouth, announce “cords visualized,” and slide the flexible, plastic endotracheal tube into the airway. While the intern then held the tube, Angela removed the stylet, a thin metal rod placed in the ET tube to provide a degree of rigidity during the intubation process. Affixing the Ambu to the top of the ET tube, she handed it to the intern so he could continue breathing for the patient while she injected a small amount of air into the tube’s cuff. The cuff is a small ballon (a seal) affixed near the end of the tube to protect the lungs from any debris falling in now that the usual defense mechanism, the epiglottis, is being held open by a tube.
Next, she attached a device known as a tube tamer to the ET tube and around the back of the patient’s neck to secure the device in place. With these duties complete, Angela took the Ambu back from the intern and began to smoothly and evenly compress and release it, providing ventilation for the paralyzed patient. It was at this point that Dr. Powell fixed on me with, “You, come here.”
I fully expected this would be the point where Ned would pipe up and explain to the doctor that I was new — brand damn new — and it would be best if I just watched and learned this time. Looking first to my left then right I realized that good ol’ Ned was nowhere to be found! And neither was just about anyone else. With the excitement over, the crowd had melted back into their morning rounds, the coffee shop, or the next bit of excitement in the MTC ER. Freeing my feet from the wet cement of terror that was holding them securely to the floor, I made my way to the head of the bed.
* * *
After barking me to attention, Dr. Powell had left the room, and I was alone with the intern and Angela. I managed to get my 6-foot frame under and over lines, wires, and then Angela, still bagging the patient just as easy as you please, handed me the Ambu.
“Remember, it’s in for one. Just enough volume to see the chest rise. Out for four. Let him exhale. Oh, and don’t screw up the tube,” she said. Clutching the Ambu, eyes flitting wildly between the clock — “in for one” — and the rise and fall of the patient’s rib cage — “out for four” — I watched, squeezed, counted, sweated, and prayed as Angela and the intern made their way out of the room, leaving me alone with my first-ever patient.
I can’t say for sure how long it lasted. While it seemed like an eternity, I’m sure it was only a minute or two before I was pulled back to reality by words that I will remember to my dying day: “Cess now?”
Taking precious seconds away from watching my patient’s sternum rise and fall and the second hand march around the clock face, I peered over my glasses to see who had spoken. Standing on the other side of the patient was the guy central casting would send over if you were looking for someone to play “distinguished doctor,” complete with iron-gray hair; a perfectly trimmed mustache; a crisp, white lab coat; and, most importantly to me, a nametag with a bright green stripe across the bottom that said “DOCTOR” in big, black, beautiful letters! Here was my knight in shining armor! I wasn’t going to kill the poor wretch lying on the stretcher after all! There was only one problem: It appeared I had lost the ability to understand the spoken word. I had no idea what the man was saying!
At this point, as the doctor was starting to get the drift that I wasn’t completely in control of the situation, he looked at me and repeated, “Cess now?” Processing the limited amount of data available to me, I pondered my options and took the only course of action I could think of when confronting someone who was obviously communicating in some foreign, and perhaps otherworldly, language. I spoke English loudly and slowly.
“Doc,” I said, “I don’t know who you are or what you want, but you’re a doctor, and you’re not leaving this room until someone else comes in to take over bagging this patient.” Appearing to think discretion was indeed the better part of valor — and that it might be wise to have a little backup when dealing with the apparently unbalanced RT student in ED 34 — Dr. Abidi started edging toward the door. Just a step or two from the hallway, he backed into none other than good ol’ Ned! All smiles, my wayward preceptor greeted the physician and then looked at me and said, “Where the hell have you been? They’re looking for this guy in CT scan!”
Thoughts of homicide briefly ran riot through my mind, but the relief of having someone else assume care of the patient overcame my baser impulses. We got the patient to CT, where I actually took care of him most of the time before bringing him back to his room in the ICU — all under Ned’s watchful eye.
I learned later that several Pakistani doctors were working at MTC at the time on an exchange program, including Dr. Abidi. I would get to know the doctor somewhat over my time at Maine Trauma, and while his English was infinitely better than my Urdu, it took a fair amount of time to figure out that what he was saying that fateful day was, “I assess now?”
* * *
The years between then and now have been kind, and I’ve been extremely fortunate to work with some truly talented colleagues. I do a fair bit of teaching myself now, giving seminars for new doctors, classes for ICU nurses, and talks to pulmonary rehab patients. All of those activities are satisfying in their own right, but there’s nothing like standing at the head of the bed, calmly bagging, and making sure no one screws up the tube.

